The Role of Insulin
Insulin is a hormone produced by the pancreas, the organ that sits just behind the stomach. Insulin is released in response to food intake. Its production is stimulated most by dietary carbohydrates and least by dietary fat.
Insulin has several functions throughout the body. One of the most important is to facilitate the entry of glucose into cells to be used for energy. Almost every cell in the body has both insulin receptors and glucose receptors. The glucose receptor is totally reliant on the insulin receptor. For the glucose receptor to be open to allow glucose into the cell, the insulin receptor needs to be occupied by an insulin molecule. In this way, insulin behaves like a key to open up the cell to allow glucose in.
In the normal order of events, we eat food, which stimulates insulin production. Glucose is absorbed from the gastrointestinal system into the bloodstream. At the cellular level, insulin connects with the insulin receptor activating the glucose receptor so the glucose can enter the cell to be used as energy.
In Type 1 diabetes, the pancreas does not produce enough insulin. As a result, glucose can’t enter cells and gradually builds up in the bloodstream. Treatment involves insulin replacement via injection.
What is Insulin Resistance?
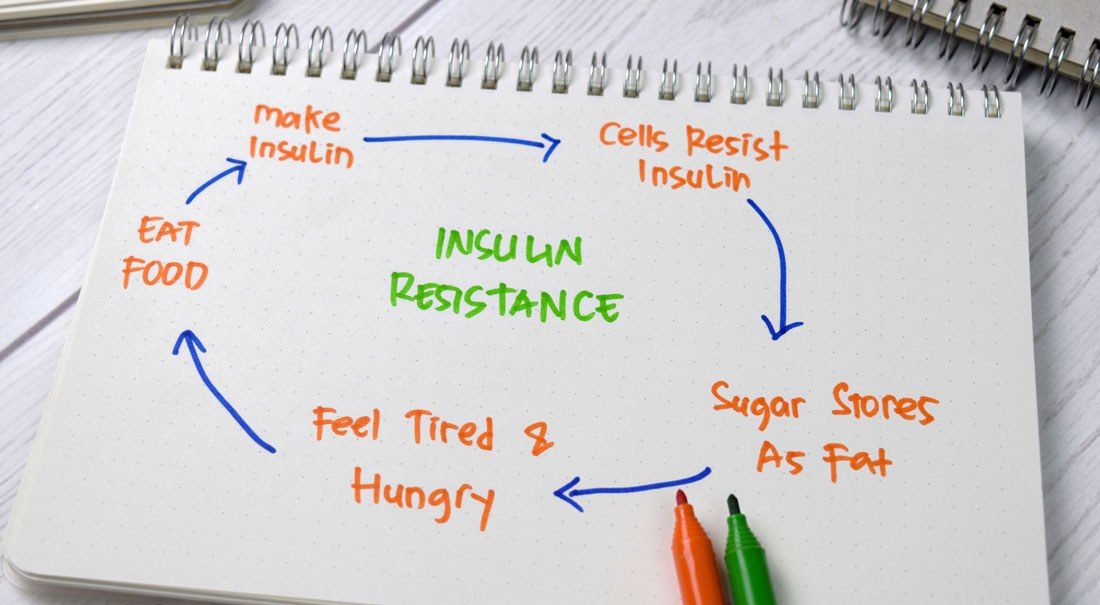
Insulin resistance is a condition where insulin is present, but its effects are resisted by the cell. The body responds by increasing insulin production, making the insulin receptor more resistant. This is the start of a vicious cycle of increasing insulin resistance and insulin production until the body eventually loses its ability to control blood sugar and Type 2 diabetes is diagnosed. The time lag between the start of insulin resistance and the diagnosis of Type 2 diabetes may be as long as fifteen to twenty years.
Insulin resistance, and the co-existing increased insulin production, induce an inflammatory state in the body and are associated with a large number of medical problems including obesity, high blood pressure, fatty liver, blood lipid abnormalities, arthritis, heart attacks, strokes, dementia and various cancers including breast, prostate and colon cancer.
Insulin resistance may be asymptomatic or induce subtle bodily changes like the development of skin tags.
The risk of insulin resistance increases if there is a family history of type 2 diabetes, obesity, lack of exercise or a high carbohydrate diet. However, the incidence of insulin resistance has soared within the last two decades. It is estimated that one in three Australian adults now suffer from insulin resistance. What has caused the epidemic of insulin resistance is unclear. Could it be our increased consumption of ultra-processed foods and seed oils or our increased exposure to environmental toxins such as pesticides, herbicides and pollution over this time period?
What is Type 2 Diabetes?
In the last two decades, the incidence of Type 2 diabetes in Australia has doubled, with about one in twenty Australians diagnosed. Furthermore, it is estimated that there is a similar number of Australians are living with diabetes but are yet to be diagnosed.
Early symptoms of Type 2 diabetes can be very subtle. As the disease progresses and blood sugars increase, symptoms such as blurred vision, excessive thirst and urination, and recurrent urinary tract infections can develop.
Left untreated, Type 2 diabetes can have devastating consequences such as:
- Stroke
- Heart attack
- Diabetic Eye disease and blindness
- Diabetic kidney disease and kidney failure
- Peripheral vascular disease resulting in limb amputations
- Dementia and Alzheimer’s disease
- Early death
In general, treatment involves medications which are increased and expanded as the diabetes gets worse with time. The majority of patients will end up using injectable insulin.
Managing Type 2 Diabetes with Diet
Until very recently, we believed that Type 2 diabetes was an unrelenting progressive medical condition. We now know, however, that in many cases, Type 2 diabetes can be put into remission with a low carbohydrate diet.
All major international diabetes associations, including Diabetes Australia, acknowledge this position statement for low carbohydrate eating for people with diabetes.
A low carbohydrate diet decreases the elevated blood sugar, the high insulin levels, and the underlying insulin resistance. With time this can lead to better diabetic control, lower blood pressure and a reduction in medication requirements. In some patients, it can lead to remission of their type 2 diabetes.

References
Effectiveness and Safety of a Novel Care Model for the Management of Type 2 Diabetes at One Year: An Open Label, Non-Randomized, Controlled Study. Hallberg SJ, McKenzie AL, Williams P, et al. Diabetes Therapy. 2018. DOI: 10.1007/s13300-018-0373-9 https://pubmed.ncbi.nlm.nih.gov/29417495/
Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: an open label, non-randomized, controlled study. Bhanpuri, N.H., Hallberg, S.J., Williams, P.T. et al. Cardiovasc Diabetology 17, 56 (2018) DOI:10.1186/s12933-018-0698-8 https://pubmed.ncbi.nlm.nih.gov/29712560/
Long-Term Effects of a Novel Continuous Remote Care Intervention Including Nutritional Ketosis for the Management of Type 2 Diabetes: A 2-year Non-randomized Clinical Trial. Athinarayanan SJ, Adams RN, Hallberg SJ, et al. Frontiers in Endocrinology. 2019; 10:348. DOI: 10.3389/fendo.2019.00348 https://www.frontiersin.org/articles/10.3389/fendo.2019.00348/full
Low-Carbohydrate Diets in the Management of Obesity and Type 2 Diabetes: A Review from Clinicians Using the Approach in Practice. Kelly, T., D. Unwin, and F. Finucane. International Journal of Environmental Research and Public Health, 2020. 17(7). https://www.mdpi.com/1660-4601/17/7/2557
